Do common contraceptives increase exposure to HIV?
A new study shows that the use of loop, Jadelle or Norplant and Depo Provera does not put women at a higher risk of HIV infection, Our Contributor JOSOPHINE CHINELE unpacks the new science.
By 1.50pm on June 13, the evidence for contraceptive options and HIV outcomes (Echo) at the 2019 South African Aids Conference YouTube live stream session had over 350 people already signed in.
Eager to hear the results of the new study, 11 Malawian journalists and three advocates were part of this audience, gathered at Pakachere Institute of Health and Development Communication in Blantyre.
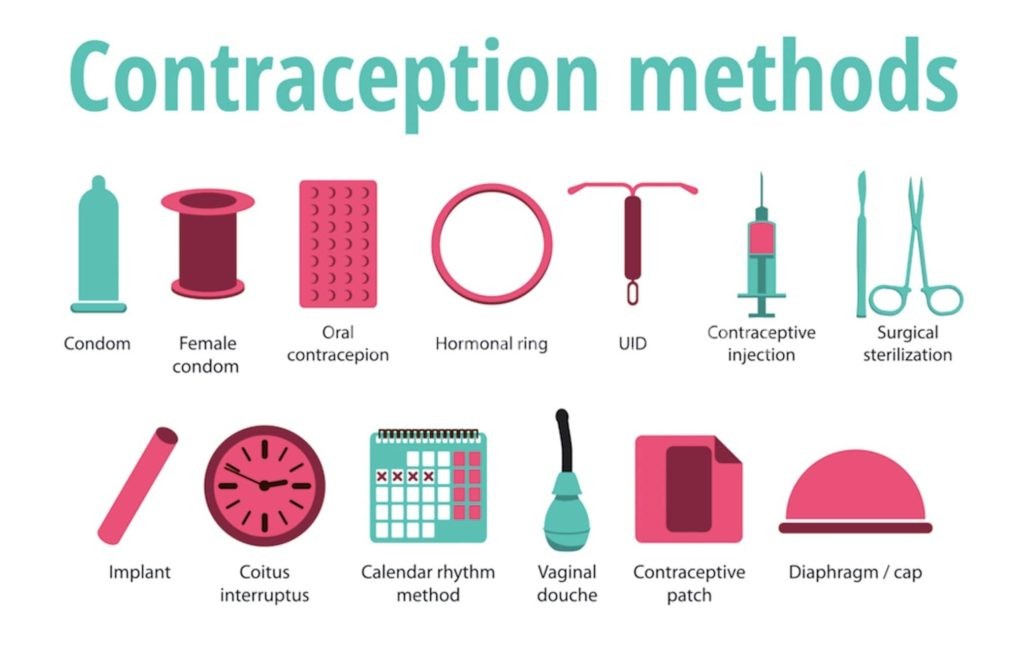
From December 2015 to October 2018, researchers compared the risk of acquiring HIV in women who used different contraception methods. Specifically, they looked at three forms of birth control—the copper-releasing intrauterine device (Cu-IUD or loop); a levonorgestrel (LNG) implant (Jadelle or Norplant); and depot medroxyprogesterone acetate-intramuscular (DMPA-IM or Depo-Provera).
“This well executed randomised trial did not find a substantial difference in HIV risk among the methods evaluated—and all [contraceptive] methods were safe and highly effective,” announced Professor Jared Beaton, from Washington School of medicine and Public Health.
A silent sigh of relief was noticeable in the boardroom.
The results bring to a rest the fear that some contraceptives specifically increase a woman’s risk to contract HIV.
However, while none of the three family planning methods increased HIV more than the other, overall HIV infection rates among the people taking part was high by almost 4 percent.
To the civil society advocacy working group on hormonal contraceptive methods and HIV, the findings are critical to women everywhere.
According to the international civil society movements, the results are particularly encouraging to young women in East and Southern Africa, including Malawi, where uncertainty around the link between DMPA and HIV risk has been of major concern for many years.
Before the new trial, epidemiological and laboratory studies have tried to determine whether there is truly an increased risk of HIV infection associated with use of hormonal contraception, according to head of Sexual and Reproductive Health and Adolescent Child Health Research Programme in Kenya, Dr Nelly Mugo.
She said, a deeper analysis of all the data across time showed that the magnitude of increased HIV risk was approximately 40 to 50 percent.
The Echo study was conducted in Zambia, Eswathini, Kenya and South Africa to finally determine whether this increase was true or not.
The four countries were selected because women in southern and eastern Africa continue to be among the hardest hit by HIV and maternal mortality.
DMPA-IM, an injectable method locally known as Depo Provera, is also the most widely used modern contraception in the country and the rest of the region.
The researchers felt it was important to work with affected communities to ensure the study provides evidence on the population most in need of guidance on hormonal contraceptive use and the possible link with HIV acquisition.
Doctor Mugo told the conference: “Some observational data indicated that Depo had some risk because high HIV incidences happened to be in areas where this method was also highly used.
“IUD was used as a non-hormonal comparator while Jadelle was included to represent progestin based contraceptive.”
In its alert to advocates, Avac—a US organisation that works in HIV prevention, says the ECHO results must prompt action.
The statement reads in part: “Now is the time for investment in woman-centered programmes that offer a full range of contraceptive choices and HIV prevention strategies at the same site and in the context of a true informed-choice approach.
The ECHO results tell us this is the case. The women who made the trial possible deserve nothing less.”
Lessons
Avac notes that even though there were high HIV incidence rates in all three arms of the trial, it does not mean that the methods increased women’s risk.
The statement puts the findings in context: “These HIV incidence rates are comparable to those seen in young women in these countries in other trials and contexts. What is notable, though, is that many trials with comparable incidence rates recruited women with specific HIV risk factors, such as numbers of partners, sex work, sexually transmitted infections, etc.
“In Echo, HIV risk factors were not part of enrolment criteria,” reads the statement in part. In the Echo study, the only sexual behavioral eligibility criterion was being sexually active. This makes the high rates of HIV infection seen in this general population alarming.
All the participants in the clinical trial were sexually active young women looking for contraception.
“ECHO gives a stark picture of the risk facing these young women. HIV prevention services must meet them where they are—in contraceptive clinics and other related services. The women in this trial are our sisters and daughters and mothers who were simply seeking contraception,” says Lillian Mworeko, executive director of the International Community of Women Living with HIV/Aids Eastern Africa.
Mworeko is also the co-chair, with Avac, of the Civil Society HC-HIV Advocacy working group in Africa.
She added: “It is a wake-up call to put HIV prevention on-site at every family planning clinic, including Pre-Exposure Prophylaxis [Prep] and female condoms with peer support and trained providers.”
Reactions
According to FP 2020 executive director Beth Schlacheter, the results are a call to work together to ensure that services are provided to the benefit of women and girls.
She said: “Women mostly get HIV or fall pregnant through sex, yet these issues have been treated separately….we know from this trial that contraceptive methods are safe and at this point you have our commitment from FP 2020 to work from what has come from Echo in the coming years,” she said.
“The key question about DMPA has been answered but that does not mean the method can continue to dominate women’s contraceptive programmes in East and Southern Africa,” said the Civil Society Advocacy Working Group
Schlacheter does not believe that DMPA should continue to be the only long acting method.
“The women, who want choices and deserve equity with high quality contraceptive programmes in high income countries,” she says.
The Civil Society working group further notes that throughout the Echo trials, the risks of unplanned pregnancy and HIV were pitted against each other by scientists and normative agencies.
Now is the time for integration. This has to include investigation, more research on how to deliver services that meet contraceptive and HIV needs well.
It’s been observed that in east and southern Africa women who need contraceptives do not have enough choice on what to use, in most cases methods like injectable are just imposed on them.
James Kiarie, coordinator of human reproduction research at the World Health Organisation (WHO), is pleased that these contraceptive methods have proven to be safe and efficient.
As WHO is planning for its a response to the new evidence, he says it has some considerations in place.
“The first one is that women and girls should have a wide choice to safe contraceptives and the second consideration is that there is need to step up HIV prevention efforts, particularly for young women and girls,” he explains.
Kiarie discloses that although the results are reassuring, the WHO will still have its experts to review the results in its entirety to revise recommendations to countries.
“WHO will also support countries to strengthen their HIV and sexual reproductive health integration. We will have a meeting with 14 high burdened countries where all these issues will be discussed,” he says. n
Josephine Chinele is a Biomedical HIV prevention Advocate, 2019 AVAC fellow working for Pakachere Institute of Health and Development Communication