TB fight goes to vulnerable communities
Tuberculosis (TB) is still the most deadly infectious disease in the world, killing over 4 000 people every day, according to the World Health Organisation (WHO).
As such, in compliance with the latest WHO Latent TB Infection (LTBI) guidelines, in 2020, the Ministry of Health rolled out short-course rifapentine-based TB Preventive Therapies (TPT) nationally as one way of providing equitable access to TB preventive therapy to all those eligible.
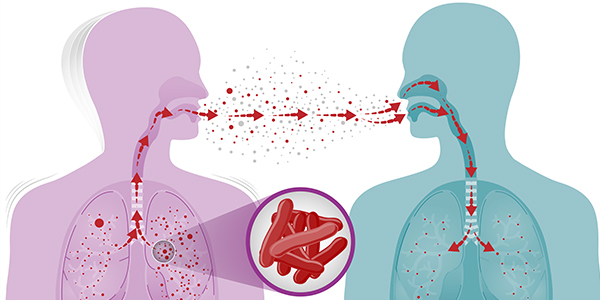
Latent TB infection means that not everyone who is infected with TB immediately develops the TB disease. Some people go on to have a dormant form of TB that can be reactivated over time or when the immune system is suppressed. So treating LTBI will prevent the person from getting active TB.
However, most people in rural areas are still not aware of how they can access the treatment. To complement government’s efforts in responding to WHO’s call to accelerate TPT provision to eligible people, the Coalition of Women Living With HIV and Aids (Cowlha) is implementing interventions in Mzimba North and Mangochi, reaching out to TB household contacts, under-five children and adolescents.
The interventions have helped people get diagnosed of TB, which has enabled them to get treatment on time.
One of such person who has benefitted from the interventions is Edna Nyasulu from Mzuzu, who says for a couple of months, she used to develop swollen legs and frequently losing appetite.
“But I had no idea about what was going on in my body. Until when Cowlha, which was conducting door-to-door visits, reached out to me,” she says.
Nyasulu states that she was encouraged to go to the hospital where she was diagnosed with TB of the lungs and she was put on treatment.
“I am now better as I am into second month of taking 3HP alongside other drugs,” she says.
According to Nyasulu, she already suspected that she was developing TB before Cowlha’s interventions.
“But I was afraid because I heard that TB dosage takes six months to complete, bringing adherence challenges in the process,” he says.
Accelerating TB fight
Through Treatment Action Groups (Tags), Cowlha, with funding from Impact 4TB, wants to see that from February 2023 to December 2023, there is an improved uptake of short course TPT regimens 3HP and 1HP for children and household contacts, by engaging communities in identifying households contact for TB to be referred for services.
The 3HP is a short-course TPT regimen which is endorsed by WHO. It combines high dose Isoniazid (H) and high dose rifapentine (P) once a week for three months. 3HP is associated with higher rates of treatment completion than isoniazid preventive treatment which TB infected patients have been taking.
According to WHO, less than 20 percent of the 37 million people living with HIV have ever started TPT due to various reasons, including ignorance. To enhance community treatment literacy efforts, especially TPT treatment literacy, the organisation equipped expert clients with skills to collect data at community level.
The expert clients conduct community sensitisation meetings as part of enhancing community treatment literacy efforts. They also conduct door-to-door visits to increase enrolment on TPT for children and household contacts.
The expert clients collect data using Community Led Monitoring (CLM).
Mangochi Cowlha district coordinator Nelly Kandulu says the expert clients have reached out to 4 800 people, mostly from support groups with messages on TPT.
“Apart from support groups, we move around in the communities with support from traditional leaders to sensitise them about TPT. The campaign is having an impact as demand for the TPT in health facilities is increasing,” she explains.
According to Davidson Maduka, a healthcare provider from Mangochi, during anti-retroviral treatment (ART) clinics, they now encounter some clients demanding for TPT, which was not the case before.
“However, it is sometimes difficult to sustain the demand due to stock outs,” he says.
Maduka, who is also a TB focal person for the district and operates from Nancholi clinic in the district, says together with Cowlha, they plan to conduct more awareness campaigns to reach out to more people.
He says those who started taking 3HP have not reported any side effects or any problem.
However, many people, especially those not in support groups, are afraid to go for TB screening as being found with TB is often associated with being HIV positive.
“This breeds stigma,” says Judith Mkandawire from Mzuzu.
Apart from conducting community sensitisation meetings, the expert clients also follow up on those newly initiated on anti-retroviral therapy (ARTs) and TPT to reduce the fear of pill burden. The experts also conduct door-to-door campaigns to identify children and household contacts to link them to care.
Cowlha executive director Edna Tembo says as the campaign moves forward, there is need to provide further guidance based on research on eligibility of breastfeeding or pregnant mothers regarding taking TPT as this remains a grey area.
She explains: “Apart from creating demand for TPT through community sensitisation, there is a need to sustain that demand through adequate stocks of commodities as stock outs often frustrate recipients who usually cover long distances to access treatment.
“There is also a need to continuously build capacity of healthcare providers on the same. In this regard, concerted efforts are required from all stakeholders and not just the government alone if we are to realise our ambitious target of ending TB by 2030.”
Tembo says Cowlha continues to contribute towards the CLM process as this is a great tool to collect qualitative and quantitative data which will provide evidence-based information, including from the recipients, to improve HIV/TB services.






One Comment