Funding slows Malawi’s plan on antibiotics
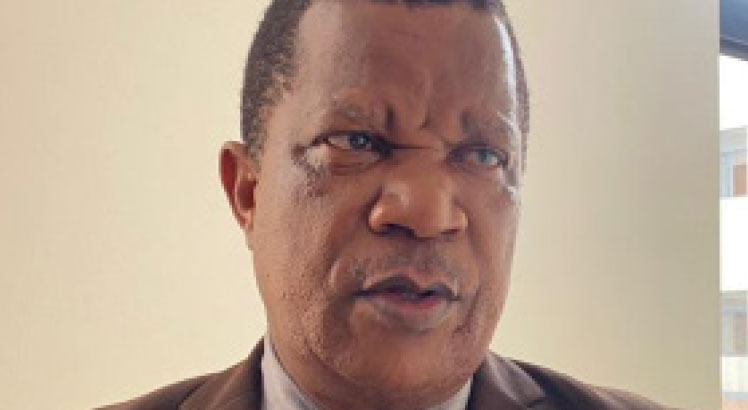
WHO estimates that 1.27 million deaths globally are attributable to resistance to antibiotics, technically known as Anti-microbial resistance (AMR), making it one of the leading causes of death. The figure is highest in countries such as Malawi, where misuse of antibiotics is common. There is free-for-all access to antibiotics without prescription. This month, the World Health Organisation (WHO) has released a report which shows that Malawi has not really achieved much on its five-year [2017-2022] national plan to manage AMR. Our Assistant Bureau Chief SUZGO CHITETE engaged the national coordinator for AMR in the Ministry of Health DR. WATIPASO KASAMBARA to shed more light on this.

Q WHO has stressed the need to increase domestic funding for implementation of AMR activities, would you share with us the funding trend since 2017/18?
A Since the establishment of the national coordinating unit on AMR within the Public Health Institute of Malawi, The country has made remarkable strides in implementing the NAP activities. However, over 90 percent of the financial support for AMR activities is donor based. Malawi government started funding AMR activities from 2017/2018 fiscal year until now, however the funding is still very minimal and it is less than $28 000 each fiscal year. Malawi has been listed among the first countries to itemize AMR in the national budget. External partners including Fleming Fund, Africa CDC, ESCA-HQ, CHAI and WHO have been key in providing support over the implementation of the Malawi AMR strategy. Overall, the support has not been sufficient enough which has led to the delays in achieving the goals outlined in the NAP.
Q Malawi needs $1 million annually for AMR activities, according to this report. How do you convince someone that this is a necessary investment in the face of so many competing priorities?
A As a country Malawi may not, at this point, support all these activities within its means due to the economic situation that the country is in, yet these activities must be prioritised in order to curb the spread of resistance infections which may cost the country more should we not act now. Notwithstanding the fact that the country is also heavily burdened with sanitation and hygiene issues, poor water sources for drinking and the burden of infectious diseases such as HIV and Aids, STIs TB, malaria, among many others, which double the risk of resistance infections. There is need to act and the time is now hence the call for support to scale up the current activities and plan for more.
Q Malawi launched a national action plan on AMR in 2017 which expires this year, how do you rate implementation?
A Malawi has managed to push towards 50 percent of the NAP implementation. The establishment of the multi-disciplinary, multi-sectoral secretariat has been the greatest achievement which has seen a well-structured governance and a well-coordinated NAP implementation. For example, on awareness, the AMRCC (AMR cordinatin committee) has managed to consistently engage the media, communities, local leaders, religious leaders, farmers, pharmaceuticals, retail and wholesale pharmacies and academic institutions on AMR and the need to rationalise the use of antibiotics. The medical practice regulatory boards have also been engaged. There are 15 operational laboratories which have been capacitated to run and effectively diagnose microbial infections. The system is operating on one health approach and currently there is a good flow of data into the central data warehouse. Our work has informed the essential drug list, review of the Malawi standard treatment guidelines, and further assisted in categorisation of antibiotics using the WHO AWARE categorisation. This promotes optimal use of antibiotics. The country has also conducted an active surveillance in poultry farms and environment. The findings are interesting yet alarming. There are several studies which are currently being done by different stakeholders through the AMRCC.
Q In 2019 WHO estimated that I.27 million deaths related to AMR occurred globally how many for Malawi?
A Malawi has not yet described the burden of AMR, but the data shows that there is a huge crisis that should soon be accounted for. Coupled with this, Malawi is among the countries with the highest burden of infectious diseases. This to say that despite the unknown burden, Malawi is affected by resistance infections to a greater degree.
Q Do all district hospitals have clinical and laboratory capacity to detect drug resistance pathogens? If not how do you intend to improve this capacity?
A Improving the quality of bacteriology services has become a major driving force for changes to quality bacteriology diagnostic services in Malawi, with only about 35 percent of the laboratories having the bacteriology capacity. Generally, the other laboratories can improve with provision of appropriate trainings (skills improvement) to the staff, required equipment and quality laboratory reagents and consumables.n