No time to dose off
A clinician’s sleepless nights bring to light huge sacrifices health workers are making to ensure no one dies of cholera, our Staff Writer JAMES CHAVULA writes:
A sweltering Tuesday in December. A cyclist, from Senjere Village near Ngala fishing hotspot in Karonga, wheels a frail fisher with sunken eyes into Nyungwe Health Centre. The 25-year-old in agony went fishing in Lake Malawi the previous day. This evening, he is vomiting and purging profusely.
It turns out this is cholera, which has taken ill 821 Malawians and killed 25 in 13 districts.
The outbreak has left overwhelmed health workers such as Martin Banda with no time to rest.
“Since the first cholera patient arrived on December 12 last year, there has been no time to dose off,” says the clinician in charge of the health centre. “We worked day and night to save patients. So far, we have handled 108 cases out of over 345 the district has registered. Sadly, we lost three: one died at home, another on arrival and the other in the treatment camp.”
Banda and his team are among health workers making huge sacrifices to treat people hit by the infectious sanitation-related disease countrywide.
In February, Parliament stuttered to a brief pause as Minister of Health Atupele Muluzi led a minute of silence in memory of the lives that have been lost to cholera and to thank selfless healthcare professionals working hard to care for patients.
“Their care and hard work has made a significant difference to those who have contracted the disease and has been instrumental in saving the lives of many,” he said.
At Nyungwe, a skeletal workforce—the clinician, a medical assistant, three nurses-cum-midwives, one community midwife and 21 health surveillance assistants (HSA)—have been overstretched by the outbreak first noted on November 24 2017 in Kaporo on the northern tip of the border district.
The disease burden has forced them to split into two teams, each comprising a clinician, nurse and an HSA.
Banda explains: “We had to act fast and strategically to avoid creating gaps in our everyday work and that all patients are assisted accordingly.
“When my team is in the cholera treatment camp, the medical assistant’s team attends to the outpatients department where we see no less than 250 patients daily. We take turns in the cholera treatment camp, some taking daytime shifts and the other at night.”
Last week, the treatment camp at Nyungwe spanned four days without a cholera patient.
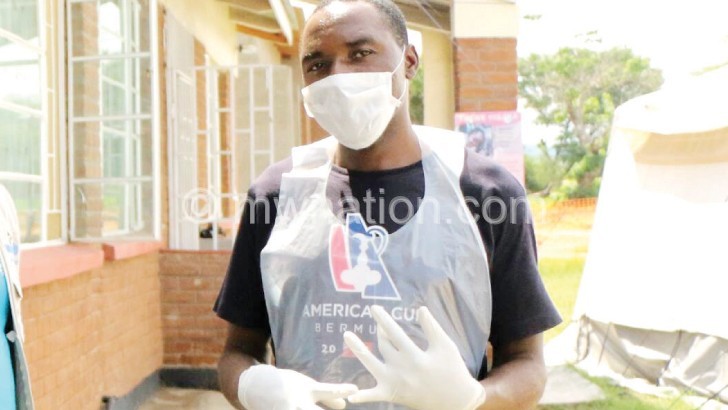
The health workers, who sometimes worked without gloves due to unexpected stock-outs, are optimistic that the outbreak is on the wane.
Banda, 36, says he cannot wait to spend some free time with his wife and three children.
He offers flashbacks of the increased workload the health workers, already burdened by cases of malaria, diarrhoea, respiratory infections and other everyday infections, had to bear.
The setting is a cordoned-off cholera camp. Cholera is highly infectious, so not even health workers and guardians step into the high risk zone without gloves, masks, gumboots and aprons. At the entrance is a blanket soaked in concentrated chlorine to reduce the risk of transmitting germs from the tent to the rest of the population.
“On the busiest day, we had 12 patients at once and two had arrived in a life-or-death condition. They were severely sick that they needed one-litre intravenous drips, one after another. I was on call. It was raining heavily. We were getting soaked, but we still had to take care of the patients. If we didn’t do so, they would have died,” says Banda.
They survived, an elating triumph which compensates for the care providers’ heartaches of spending days and nights away from their families.
“My wife and children really missed me. They rarely had time with me as I spent more time in the cholera camp. But ours is a calling to save lives first,” reasons Banda.
His major heartbreak?
“Death of a patient on a path to recovery,” he explains. “A health worker is a human being like any other. We want patients to go home feeling better. When they get well, we celebrate with them. When they die, we grieve and the sense of loss can be devastating.”
Banda admittedly wept the day a five-year-old, from Gumi, died in the treatment camp. He recalls: “The child had sepsis as well. We did our best to treat the co-infection first so that we could treat cholera without delays.
“She was getting better and I went home in the dead of the night, believing she would survive. Suddenly, she developed severe diarrhoea in the wee hours. Walking back to work in the morning, a workmate phoned me that she had died. My feet fell cold. I couldn’t walk. Tears rolled down. She died just when we thought she was safe.”
The girl is one of seven people who have died of cholera in Karonga, where the prevailing outbreak started five months ago.
The district has registered 348 cases and seven deaths, the highest count per district.
According to Ministry of Health spokesperson Joshua Malango, 31 patients were still in camp in all affected districts where health workers were hard at work.
Trends of infection show the outbreak originated from Kyela Town in neighbouring Tanzania, says Karonga district health officer Lewis Tukula.
Early patients included cross-border businesswomen who went there to order goods and might have taken food or water in the town, he explained.
Says Banda: “The numbers are dropping in daily, but we are still on high alert just in case….” n